aNewDomain — Almost a century ago, in 1922, Ukrainian pathophysiologist Alexander Bogomolets proposed that the deterioration of the connective tissues cause aging.
aNewDomain — Almost a century ago, in 1922, Ukrainian pathophysiologist Alexander Bogomolets proposed that the deterioration of the connective tissues cause aging.
In his later work [1], he stated that “A person has the age of his/her connective tissue.”
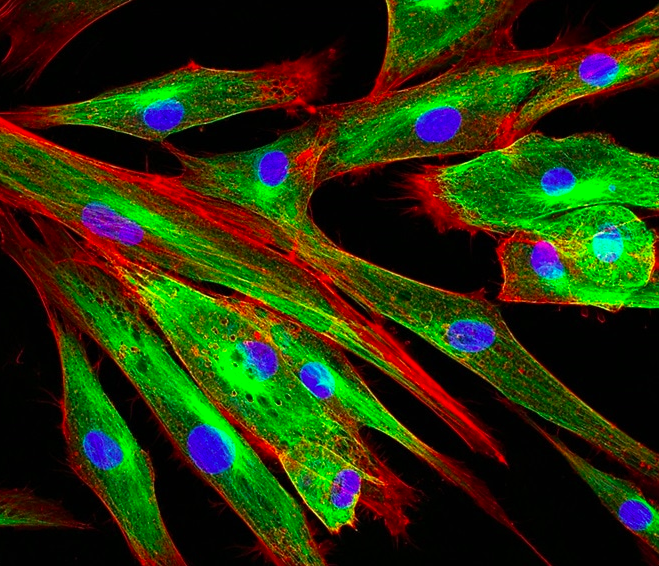
Connective tissue includes fibrous tissues, fat, cartilage, bone, bone marrow, blood, and embedded in a significant amount of extracellular materials.
Varied types of collagens constitute the main component of the connective tissue of vertebrates and make up about one-third of the body’s protein content.
The impact of extracellular matrix proteins cross-linking on the aging process and aging-related diseases was studied in the early works of Johan Björksten, which date back to 1942. The author proposed that the formation of intra- and intermolecular covalent cross-links changes the structure of the macromolecules and leads to their dysfunction [2]:
“The aging of living organisms I believe is due to the occasional formation, by tanning, of bridges between protein molecules, which cannot be broken by the cell enzymes. Such irreparable tanning may be caused by tanning agents foreign to the organism, or formed by unusual biological side reactions, or it may be due to the formation of a tanning bridge in some particular position in the protein molecules. In either event, the result is that cumulative tanning of body proteins, which we know as old age.”
Fritz Verzár demonstrated in the 1950s for the first time that the age-dependent modifications of the extracellular matrix exponentially increase the cross-linking of collagen fibers [3].
These modified proteins remain unrepaired, accumulate throughout a person’s lifetime, and cause changes in mechanical properties of a niche microenvironment, tissues, and organs, which leads to a vicious cycle of progressively increasing damage, and limits the application of senolytics, the stem cells, and other “anti-aging” therapies.
Need for Research
To date, there is not one modern method which discusses the connection between life expectancy and factors such as exosomes of stem cells, donor mitochondria, senolytics, epigenetic rollback (the list can be continued), is able to restore the structure of the extracellular matrix, the mechanical properties of which are no less of an important feature than the chemical signaling factors (through ions and molecules) in determining the fate of a cell, tissue, organ and organism as a whole.
Moreover, molecules of collagen contain a large amount of proline, an amino acid which can conduct weak electromagnetic waves generated by both the cells and tissues. Therefore, one cannot exclude the possibility that connective tissue, as well as other mechanic and electric signals, form an integrated bioelectric signaling system in the body.
It is interesting to note several works in which researchers, by changing the environment topography [4, 5] and electromagnetic radiation [6, 7], were able to not only control the cell fate but also change adult somatic cells into stem cells without the help of viruses with Yamanaka factor vectors.
Even minor structural changes in the extracellular medium affect gene expression and cell function. Both, mechanical signals transmitted through the cytoskeleton of the cell and the rigidity of the nuclear lamina jointly regulate the dynamics of the nucleus and chromatin [8, 9].
So, “young” fibroblasts age in the old matrix and vice versa — “old” cells lose the signs of the secretory phenotype associated with aging in the “young” matrix [10–12].
Also, it is likely that the mechanical properties of the extracellular matrix affect the morphology of mitochondria and the synthesis of ATP [13–14].
While some may speculate that if the old matrix is destroyed, the body updates the collagen and creates a new and more improved version of the previous matrix. However, they would be ignoring the fact that according to several studies, skin collagen molecules have a half-life of 15 years, while cartilage has a half-life of over 100 years [15–17] as well as the restrictions of the process — there are currently no selective enzymes, so all the proteins will have to be destroyed. Furthermore, upon increasing the number of cross-links, collagen fibers become denser making the matrix less accessible for the enzymes which take part in the natural circulation of collagen. Consequently, the speed of protein turnover in the matrix slows down with time resulting in further cross-links.
The process of glycation (the cause of cross-links) is practically unregulated. There is the possibility of containing glycation through transglycation [18], during which glutathione, polyamines, thiols, free amino acids (e.g., taurine and lysine) are consumed, preventing the formation of new crosslinks. Additionally, there is the possibility of limiting the damage of the body’s response to an increase in the rigidity of the matrix — secretion of transforming growth factor-beta (TGF-beta), Cysteine-rich angiogenic inducer 61 (Cyr61/CCN1) and other signaling molecules. For example, tissue fibrosis can be slowed down by inhibiting matrix metalloproteinases, one of which is doxycycline.
Unfortunately, even with the emergence of David Spiegel’s promised solution [19], whose group is working on creating enzymes against glucosepane (one of the most abundant crosslinking products in the human body), the problem is still not solved — destruction of one of about 20 types of known crosslinks will most likely be temporary so will not significantly change the mechanical properties of the extracellular matrix.
In addition to covalent crosslinking, the long-living proteins are also aging because of spontaneous racemization of aspartic acid residues [20–22].
Upon increasing the number of cross-links, collagen fibers become denser, making the extracellular matrix less accessible to enzymes (such as L-isoaspartyl methyltransferase [23]) that restore those structurally altered by the racemization of amino acid proteins under normal conditions [24]. This contributes to the accumulation of damaged proteins in collagen, which adversely affects the mechanical strength of tissues during aging [25].
Therefore, besides the destruction of extracellular matrix crosslinks, it is necessary to find a solution to accelerate the recovery of proteins, which are altered by the racemization of amino acids.
Understanding the consequences of the formation of protein crosslinks requires more attention both from the scientific community and independent researchers who are passionate with regards to the extension of the human lifespan.
By doing so, it allows us to level up the playing field where we can create and work on more serious and impactful solutions.
Cover image rendition of extracellular matrix proteins: via News.Medical.Net, Vshivkova/Shutterstock.com
References:
1. Frol’kis, V.V., [The development in modern biology of A.A. Bogomoletz’ ideas on aging]. Fiziol Zh, 1971. 17(3): p. 352–6.
2. Bjorksten, J., Some Therapeutic Implications of the Crosslinkage Theory of Aging, in Protein Crosslinking: Nutritional and Medical Consequences, M. Friedman, Editor. 1977, Springer US: Boston, MA. p. 579–602.
3. Robert, L., An original approach to aging: an appreciation of Fritz Verzar’s contribution in the light of the last 50 years of gerontological facts and thinking.Gerontology, 2006. 52(5): p. 268–74.
4. Steward, A.J. and D.J. Kelly, Mechanical regulation of mesenchymal stem cell differentiation. J Anat, 2015. 227(6): p. 717–31.
5. Roy, B., et al., Laterally confined growth of cells induces nuclear reprogramming in the absence of exogenous biochemical factors. Proc Natl Acad Sci U S A, 2018. 115(21): p. E4741-e4750.
6. Levin, M., Reprogramming cells and tissue patterning via bioelectrical pathways: molecular mechanisms and biomedical opportunities. 2013. 5(6): p. 657–676.
7. Baek, S., et al., Electromagnetic Fields Mediate Efficient Cell Reprogramming into a Pluripotent State. ACS Nano, 2014. 8(10): p. 10125–10138.
8. Makhija, E., D.S. Jokhun, and G.V. Shivashankar, Nuclear deformability and telomere dynamics are regulated by cell geometric constraints. Proc Natl Acad Sci U S A, 2016. 113(1): p. E32–40.
9. Kirby, T.J. and J. Lammerding, Emerging views of the nucleus as a cellular mechanosensor. Nat Cell Biol, 2018. 20(4): p. 373–381.
10. Chen, X.D., Extracellular matrix provides an optimal niche for the maintenance and propagation of mesenchymal stem cells. Birth Defects Res C Embryo Today, 2010. 90(1): p. 45–54.
11. Choi, H.R., et al., Restoration of senescent human diploid fibroblasts by modulation of the extracellular matrix. Aging Cell, 2011. 10(1): p. 148–57.
12. Block, T.J., et al., Restoring the quantity and quality of elderly human mesenchymal stem cells for autologous cell-based therapies. Stem Cell Res Ther, 2017. 8(1): p. 239.
13. Bartolak-Suki, E., et al., Regulation of Mitochondrial Structure and Dynamics by the Cytoskeleton and Mechanical Factors. Int J Mol Sci, 2017. 18(8).
14. Bulthuis, E.P., et al., Mitochondrial morphofunction in mammalian cells.Antioxid Redox Signal, 2018.
15. Verzijl, N., et al., Effect of collagen turnover on the accumulation of advanced glycation end products. J Biol Chem, 2000. 275(50): p. 39027–31.
16. Heinemeier, K.M., et al., Lack of tissue renewal in human adult Achilles tendon is revealed by nuclear bomb (14)C. FASEB J, 2013. 27(5): p. 2074–9.
17. Thorpe, C.T., et al., Aspartic acid racemization and collagen degradation markers reveal an accumulation of damage in tendon collagen that is enhanced with aging. J Biol Chem, 2010. 285(21): p. 15674–81.
18. Szwergold, B.S., S.K. Howell, and P.J. Beisswenger, Transglycation — a potential new mechanism for deglycation of Schiff’s bases. Ann N Y Acad Sci, 2005. 1043: p. 845–64.
19. Streeter, M., et al., Identification of Glucosepane Cross-Link Breaking Enzymes. 2018. 67 (Supplement 1).
20. Helfman, P.M. and J.L. Bada, Aspartic acid racemization in tooth enamel from living humans. Proc Natl Acad Sci U S A, 1975. 72(8): p. 2891–4.
21. Helfman, P.M., J.L. Bada, and M.Y. Shou, Considerations on the role of aspartic acid racemization in the aging process. Gerontology, 1977. 23(6): p. 419–25.
22. Ritz-Timme, S. and M.J. Collins, Racemization of aspartic acid in human proteins. Ageing Res Rev, 2002. 1(1): p. 43–59.
23. Lanthier, J. and R.R. Desrosiers, Protein L-isoaspartyl methyltransferase repairs abnormal aspartyl residues accumulated in vivo in type-I collagen and restores cell migration. Exp Cell Res, 2004. 293(1): p. 96–105.
24. Philp, C.J., et al., Extracellular Matrix Cross-Linking Enhances Fibroblast Growth and Protects against Matrix Proteolysis in Lung Fibrosis. Am J Respir Cell Mol Biol, 2018. 58(5): p. 594–603.
25. Thorpe, C.T., et al., Aspartic acid racemization and collagen degradation markers reveal an accumulation of damage in tendon collagen that is enhanced with aging. J Biol Chem, 2010. 285(21): p. 15674–81.